Elective Single Blastocyst Transfer
Reduces the twin pregnancy rate and can improve the in vitro fertilization live birth rate.
Elective Single Blastocyst Transfer
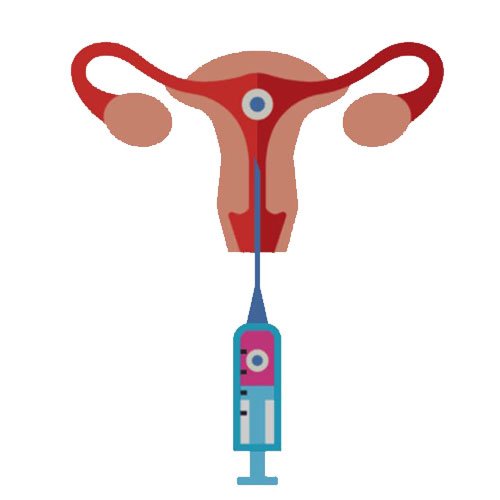
Elective Single Blastocyst Transfer (eSBT) refers to the practice of transferring a single high-quality blastocyst into the uterus during an IVF (In Vitro Fertilization) cycle, even when multiple embryos are available for transfer. This approach aims to optimize the chances of a successful pregnancy while reducing the risks associated with multiple pregnancies.
In conclusion, Elective Single Blastocyst Transfer is a strategy in IVF aimed at achieving a healthy pregnancy while minimizing the risks associated with multiple pregnancies. It requires careful consideration of factors such as patient age, embryo quality, and individual preferences, guided by discussions with fertility specialists to optimize outcomes.
Here are some key aspects to consider regarding Elective Single Blastocyst Transfer:
In conclusion, Elective Single Blastocyst Transfer is a strategy in IVF aimed at achieving a healthy pregnancy while minimizing the risks associated with multiple pregnancies. It requires careful consideration of factors such as patient age, embryo quality, and individual preferences, guided by discussions with fertility specialists to optimize outcomes.
Here are some key aspects to consider regarding Elective Single Blastocyst Transfer:
Blastocyst Development :
Blastocysts are embryos that have advanced to a more developed stage (usually around day 5 or 6 after fertilization) and have differentiated into two distinct cell types: the inner cell mass, which develops into the fetus, and the trophectoderm, which becomes the placenta. Blastocysts are generally considered more likely to implant successfully compared to earlier stage embryos.
Benefits :
Reduced Multiple Pregnancy Risk: One of the primary benefits of eSBT is minimizing the risk of a multiple pregnancy (twins, triplets, etc.), which is associated with higher risks of complications for both the mother and babies.
Improved Pregnancy Rates: Studies suggest that transferring a single high-quality blastocyst selected through criteria like morphology and genetic screening (PGT-A) can achieve comparable or even better pregnancy rates compared to transferring multiple embryos, particularly in younger women with good prognosis.